Excerpt from article in press
“Achieving Breakthrough Outcomes: Measurable ROI”
The Case Manager Official Journal of the Case Management Society of America September 2006
…Let me tell you a story. A CAD patient went to his doctor and asked, “What is cholesterol?” The doctor responded, “Oh! No problem, here’s a tear sheet from the American Heart Association.” The man didn’t understand it. He thought, “My father has CAD, too. He has a different doctor.” So he asked his father to ask his doctor the same question. The father went to his clinic. He asked his doctor, “What is cholesterol?” The doctor said, “Oh! No problem. Here you go,” and tore off the same tear sheet for the father.
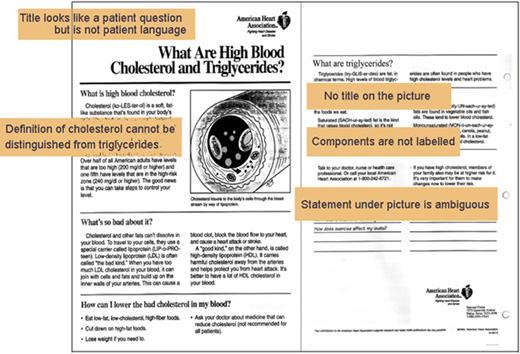
Why didn’t these men understand the handout? They were not limited literacy. Both of them ran their own businesses. They just didn’t know what cholesterol was. We all know this handout. What does it say cholesterol is? “Cholesterol is a fat-like substance.” But then it says, “Triglycerides are fat in chemical terms.” What does this mean? Is cholesterol fat or is it not fat? He didn’t ask about triglycerides. How are they different from cholesterol? The handout does not say. The title of the whole handout is a problem as well. It looks like a question a patient might ask, but what patient goes up to a doctor and asks, “Excuse me, Doctor, but what are high blood cholesterol and triglycerides?” No human being would ever ask use those words. If you are someone who doesn’t know what cholesterol is, in the title you see at once, “This handout is not going to be talking my language.”
But let’s keep going and work hard at understanding. The handout has a picture. What is this picture? What is the title? There is no title. If you don’t know what cholesterol is, you are not going to know what this picture is. But let’s keep working. The picture has some circles and some ovals. What is this big circle and what are these little ovals? There’s nothing here to tell me. There are no labels on the components. Well, at least there’s a sentence down underneath the picture. What does it say? “Cholesterol travels through the blood by way of lipoprotein.” What does that mean? Not long ago, I went to Richmond by way of Atlanta. Is “lipoprotein” a place? In terms of the Juran Quality Institute, this handout from the American Heart Association is not fit for use.
I have a friend who is an investment banker. He says, “In all my years investing in start-up ventures, I’ve learned one thing for sure: never let the engineers write the user instructions.” Unfortunately, there’s a parallel dictum: never let the clinicians write the patient instructions.
St. Joseph Medical Center in Lexington KY wanted to do something about this problem for heart failure patients, who need to know about cholesterol. They hired ethnographers who had redesigned a whole set of materials according to ethnographic research and other principles of qualitative research and evidence-based design. Here is the redesigned handout on cholesterol.
First, it uses the patients’ language, the simple question, “What is cholesterol?” as the title. Before it tells about triglycerides, it answers the question: “Cholesterol is fat.” That’s all patients need to know. They are not going to be lab researchers splitting hairs on definitions of whole blood components. “Cholesterol is fat in your blood.” Once that’s established, we take a small step the next thing we want them to know: There are actually “two kinds of fat in your blood, cholesterol and triglycerides.”
In the overall layout of the page, you see two large words, Cholesterol and Triglycerides, with text under each. At a glance you know it’s going to explain both. You’ll notice pictures, but not cutaway diagrams of body parts. What’s here are familiar images to make new concepts understandable. Finding familiar images that work for a complex clinical concept is not easy-especially because we are committed to not mixing metaphors. We will not say LDL is like one thing and HDL is like another. We search for an image of a single, familiar substance that is just like cholesterol: sticky when it’s loosely packed
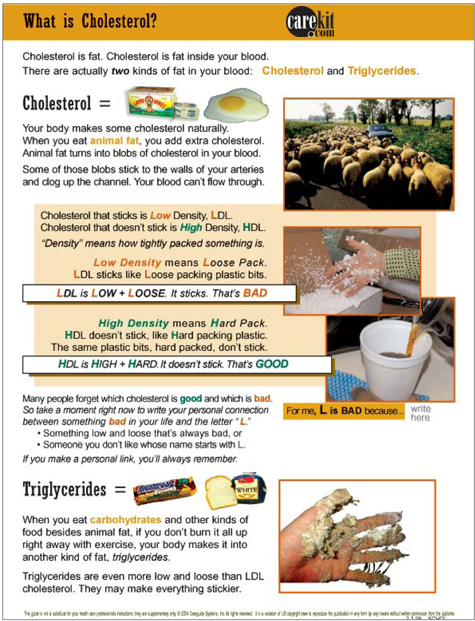
and not sticky when tightly compressed. We beat our heads on this until we came up with styrofoam. When it’s in loose little pieces, it sticks to your hands, to shipping cartons, to anything it touches. But when you compress styrofoam and make it hard, you can make all kinds of things out of it that don’t stick, like a coffee cup. Now we have an image that a person can remember and work with. You can teach effectively with it, or the person may be able to learn by extending the metaphor themselves. Why is hard-packed cholesterol good? If you take a piece of hard styrofoam, and draw it through a pile of loose styrofoam bits, the bits will stick. You can draw them right out. That’s why hard cholesterol is good; it draws out loose, sticky cholesterol.
When it comes to remembering that LDL is bad and HDL is good, even clinicians can have a little trouble sometimes. So what this material does is take a leson from industry. Consumer products experts know how to make you remember. There is, in a recent film, a sad but hilarious sidewalk interview where everyone walking by the White House can sing the Big Mac song, but none of them knows any of the Bill of Rights. As health care providers, let’s take the techniques of consumerproducts advertising and make these health care information points memorable, as intrinsically memorable as the Big Mac jingle.
Ask the patient to think of something bad that starts with L. Something or someone they don’t like that starts with L. We ask them to associate something bad with L and not something good with H, because human nature always brings shock and humor along with bad. Shock and humor will lodge the association in our memory. If you are using this material to teach, and your learner comes up with an L that is obviously bad and works for them–fine. Move on with your teaching. But if they can’t think of a bad L, start giving them hints: “There is one thing we all know that when it’s low and loose, it’s not very desirable, but when it’s high and hard-well, you want just about as much of that as you can get.”
Shock. Humor. And I guarantee you will never forget it again.
Now we get to the last point: triglycerides. What are they? There’s nothing we could find on the Web, on any patient-directed site, that tells what triglycerides actually are. Only when we dug into nursing textbooks could we find a professional description. It turns out that while cholesterol comes from animal fat, triglycerides come from eating other kinds of food. So we have a neat, tight framework for understanding the difference in their origins. Next, the textbooks said triglycerides are even lower and looser than LDL. They make everything even more sticky. I was very gratified when the medical director of one of the largest health plans in the country said, “That’s the best explanation of cholesterol I’ve ever seen.”
All of this may be entertaining, but it would have no value if it didn’t make a difference in patient outcomes. What happened in Lexington, Kentucky? This cholesterol handout was one of a set that were redesigned in similar ways for a heart failure program. The hospital measured readmission, length of stay, and length of stay on readmission. The materials that were redesigned were delivered at discharge. A DME person, familiar with the handouts, came to the house and evaluated patients’ oxygen needs, but no other follow up was provided. The hospital quality department collected the statistics. St. Joseph was already doing well with their outcomes before they started this program. Their readmission rate for heart failure was 8.6%, which was about half the national average at the time. They were one day over the Medicare limit on length of stay. For those that were readmitted, the second stay was almost 6 days of unreimbursed costs.
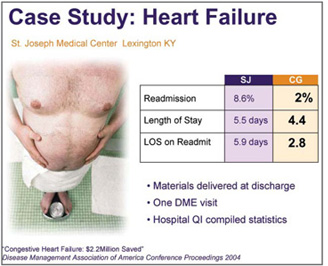 Each month of using the materials, the readmission rate dropped steadily till it reached 2%. The initial LOS went to 4.4 days. The readmission LOS shrank by half, to 2.8 days.
Each month of using the materials, the readmission rate dropped steadily till it reached 2%. The initial LOS went to 4.4 days. The readmission LOS shrank by half, to 2.8 days.
In discussions of compliance, providers seldom discuss the quality of their handouts, but often blame patients for being resistant. Interventions like St.Joseph’s suggest that if we give patients materials they can understand, the majority will spontaneously comply.
Patients are not resistant; they have received materials that are not fit for use.
Sometimes people ask if St.Joseph’s outcomes were really because of the materials. The hospital staff were doing other things, after all. When we examine the time line of the project, we see that the rate of readmission was dropping month by month after beginning the materials distribution. Then in June they shot back up again. What happened? Only one case manager had been responsible for passing out the materials. He went on vacation. No one passed out the materials.
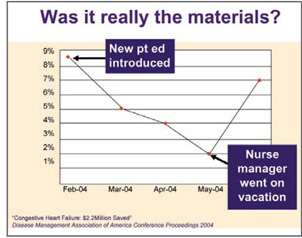 This nurse, Alan Howard, reports, “Nothing else we were doing made any difference when we took away the materials that enabled the patients to act independently.”
This nurse, Alan Howard, reports, “Nothing else we were doing made any difference when we took away the materials that enabled the patients to act independently.”
After the materials were reinstated, the rate of readmission dropped again and remained around 4% for the remainder of the year. A true breakthrough.
We don’t realize the magnitude of patients misunderstand what we write for them. Rush Medical Center in Chicago decided to measure whether patients understood their post surgical instructions for changing a dressing. For three months, they followed their normal procedure of distributing gauze and tape to patients after abdominal and orthopedic surgery. They also gave away instructions the nurses had written that were approved by the Patient Education Committee. One week after discharge, they called the patients and asked, “Were you able to manage without calling for repeat instructions or asking anyone for help?” They were astute enough not to ask, “Did you understand?” because everyone will say yes. That’s a focus-group kind of question.
Some of the patients answered, “Yes, I was able to follow the instructions.” What percentage do you think answered yes? People often guess about half, thinking of health literacy statistics: at least a third of patients at Rush would probably be “limited literacy.”
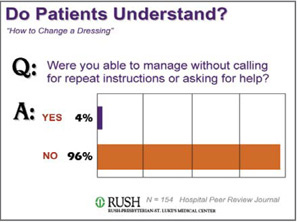 But number who answered yes was only 4%.
But number who answered yes was only 4%.
A full 96% could not change the dressing independently. Even if you take out the limited literacy population, that leaves 63% who could read and still couldn’t follow the instructions.
In no other industry would it be tolerable to have 96% failure rate. In health care, we’re not even measuring whether our patient education products work.
We write them, we get non-functional approvals, and we don’t realize that when the product reaches the context of use, it does not function.
Summary: Breakthrough in both Patient Outcomes and ROI
Whether we apply the Juran principles to patient education, to CMS pay-for-performance areas or to other quality improvement projects, the Juran Quality Improvement Cycle will earn our case management departments breakthrough ROI.
Next, get a baseline on today’s performance.
Then conduct qualitative research to learn what the functional requirements are for use in context.
From those findings, design an intervention. If measure outcomes, we have maximum freedom to consider all types of innovations.
Make sure the intervention passes all non-functional requirements.
Finally, measure the impact on outcomes—you can expect at least a 15% improvement Now begin the cycle again for another breakthrough.
If quality is fitness for use in the context of the end user, then we have no tradeoffs between ROI and patient-centered care. We can achieve breakthough in both.
